Rectal Prolapse
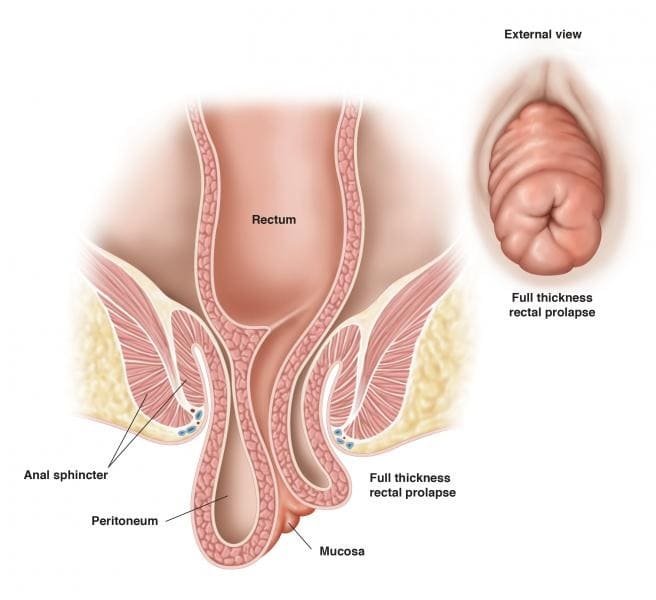
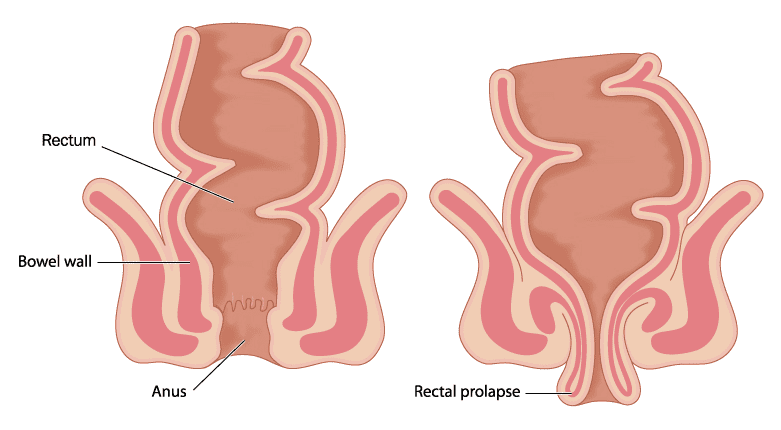
Rectal prolapse occurs when the rectum (the last section of the large intestine) falls from its normal position within the pelvic area and sticks out through the anus. (The word “prolapse” means a falling down or slipping of a body part from its usual position.)
The term “rectal prolapse” can describe three types of prolapse:
- The entire rectum extends out of the anus.
- Only a portion of the rectal lining is pushed through the anus.
- The rectum starts to drop down but does not extend out the anus (internal prolapse).
Rectal prolapse is common in older adults who have a long-term history of constipation or a weakness in the pelvic floor muscles. It is more common in women than in men, and even more common in women over the age of 50 (postmenopausal women) but occurs in younger people too. Rectal prolapse can also occur in infants – which could be a sign of cystic fibrosis – and in older children.
Causes
- Chronic (long-term) constipation or chronic diarrhoea.
- Long-term history of straining during bowel movements.
- Older age: Muscles and ligaments in the rectum and anus naturally weaken with age. Other nearby structures in the pelvis area also loosen with age, which adds to the general weakness in that area of the body.
- Weakening of the anal sphincter: This is the specific muscle that controls the release of stool from the rectum.
- Earlier injury to the anal or pelvic areas.
- Damage to nerves: If the nerves that control the ability of the rectum and anus muscles to contract (shrink) are damaged, rectal prolapse can result. Nerve damage can be caused by pregnancy, difficult vaginal childbirth, anal sphincter paralysis, spinal injury, back injury/back surgery and/or other surgeries of the pelvic area.
- Other diseases, conditions, and infections: Rectal prolapse can be a consequence of diabetes, cystic fibrosis, chronic obstructive pulmonary disease, hysterectomy, and infections in the intestines caused by parasites – such as pinworms and whipworms – and diseases resulting from poor nutrition or from difficulty digesting foods.
Symptoms
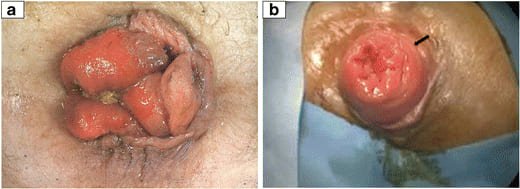
- Feeling of a bulge or the appearance of reddish-coloured mass that extends outside the anus.
- At first, this can occur during or after bowel movements and is a temporary condition. However, over time – because of an ordinary amount of standing and walking – the end of the rectum may even extend out of the anal canal spontaneously and may need to be pushed back up into the anus by hand.
- Pain in the anus and rectum and bleeding from the inner lining of the rectum.
- Faecal incontinence.
Diagnosis And Test
- Physical examination
- Anal electromyography (EMG)
- Anal manometry
- Anal ultrasound
- Pudendal nerve terminal motor latency test
- Colonoscopy
- Proctosigmoidoscopy
- Magnetic resonance imaging (MRI)
Management And Treatment
Surgery is the gold standard treatment for prolapse.
Abdominal Repair Approaches
Abdominal procedure refers to making an incision in the abdominal muscles to view and operate in the abdominal cavity. It is usually performed under general anaesthesia and is the approach most often used in healthy adults.
- Rectopexy (fixation [reattachment] of the rectum)
- Resection (removal of a segment of intestine) followed by rectopexy.
Rectal (perineal) repair approaches
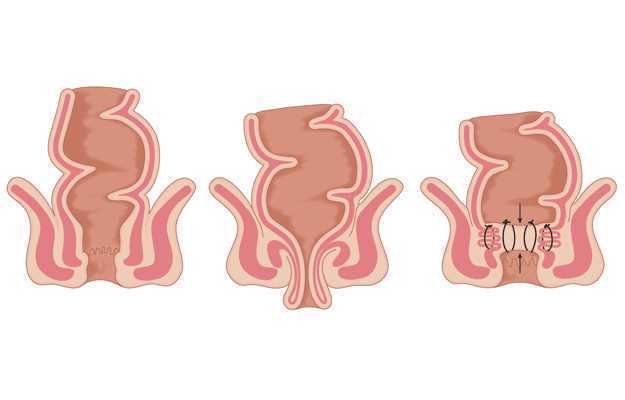
Altemeyer procedure: In this procedure — also called a perineal proctosigmoidectomy — the portion of the rectum extending out of the anus is cut off (amputated) and the two ends are sewn back together. The remaining structures that help support the rectum are stitched back together to provide better support.
Delorme procedure: In this procedure, only the inner lining of the fallen rectum is removed. The outer layer is then folded and stitched, and the cut edges of the inner lining are stitched together so that rectum is now inside the anal canal.
Risks/complications after rectal prolapse surgery
- Anastomotic Leak
- Intra-abdominal or rectal bleeding
- Urinary retention (inability to pass urine)
- Medical complications of surgery: heart attack, pneumonia, deep venous thrombosis (blood clots)
- Return of the rectal prolapse
- Worsening or development faecal incontinence
- Worsening or development of constipation
- After surgery, constipation and straining should be avoided. Fiber, fluids, stool softeners and mild laxatives can be used.
Post op Recovery
The average length of hospital stay is 2 to 3 days, but this varies depending on a patient’s other health conditions. Complete recovery can usually be expected in a month; however, patients should avoid straining and heavy lifting for at least 6 months. In fact, the best chance for preventing prolapse from returning is to make a lifetime effort to avoid straining and any activities that increase abdominal pressure.
