Pancreatitis
Overview
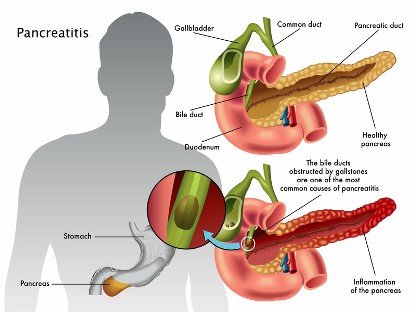
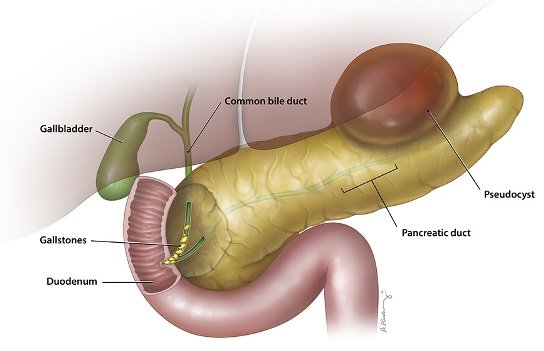
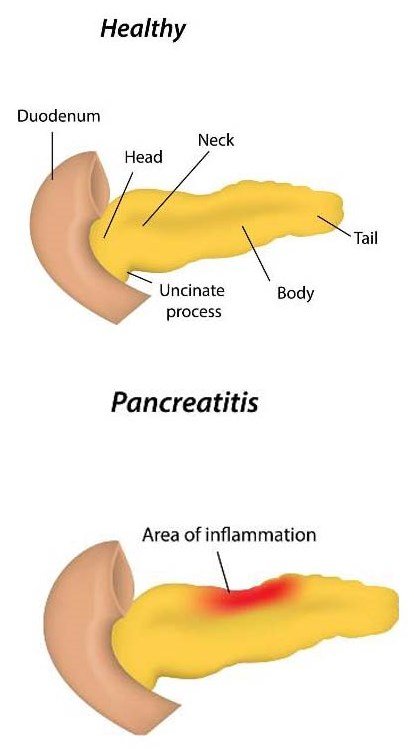
Pancreatitis is an inflammation (swelling) of the pancreas. When the pancreas is inflamed, the powerful digestive enzymes it makes can damage its tissue. The inflamed pancreas can cause release of inflammatory cells and toxins that may harm your lungs, kidneys and heart.
Types
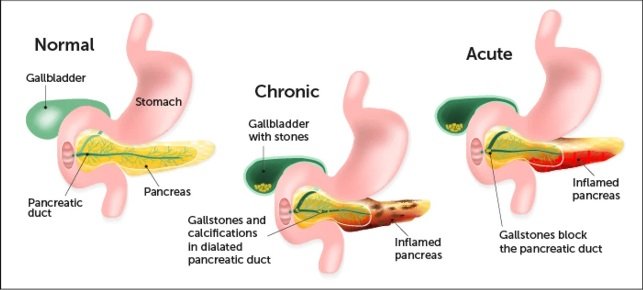
- There are two forms of pancreatitis
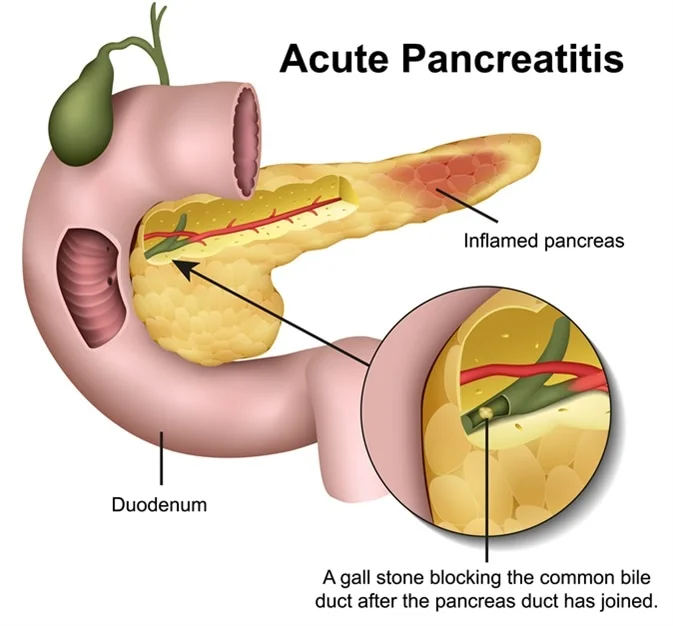
- Acute pancreatitis is a sudden and short bout of inflammation.
- Chronic pancreatitis is ongoing inflammation
Casues
Gallstones or heavy alcohol drinking are usually the cause of pancreatitis. Rarely, you can also get pancreatitis from:
- Medications (many can irritate the pancreas).
- High triglyceride levels (fat in the blood).
- Infections.
- Abdominal injury.
- Metabolic disorders such as diabetes.
- Genetic disorders such as cystic fibrosis.
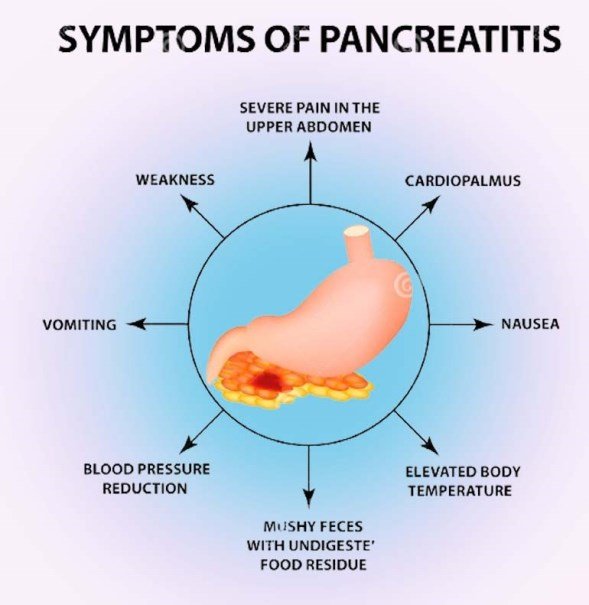
Symtons
- Acute pancreatitis symptoms
If you have acute pancreatitis, you may experience:
- Moderate to severe upper abdominal pain that may spread to your back.
- Pain that comes on suddenly or builds up over a few days.
- Pain that worsens when eating.
- Swollen, tender abdomen.
- Nausea and vomiting.
- Fever.
- Faster than usual heart rate.
- Chronic pancreatitis symptoms
Chronic pancreatitis may cause some of the same symptoms as acute pancreatitis. You may also develop:
- Constant, sometimes disabling pain that spreads to your back.
- Unexplained weight loss.
- Foamy diarrhoea with visible oil droplets (steatorrhea).
- Diabetes (high blood sugar), if insulin-producing pancreas cells are damaged.
Diagnosis
Diagnosing acute pancreatitis
For acute pancreatitis, your provider may order a blood test that measures the levels of two digestive enzymes (amylase and lipase) produced by the pancreas. High levels of these enzymes indicate acute pancreatitis. An ultrasound or computed tomography (CT scan) provides images of your pancreas, gall bladder and bile duct that can show abnormalities.
Diagnosing chronic pancreatitis
Diagnosing chronic pancreatitis is more involved. You may also need:
- Secretin pancreatic function test: This test checks for your pancreas’s response to a hormone (secretin) released by the small intestine. Secretin usually triggers the pancreas to release a digestive juice. A medical professional passes a tube from your throat, through your stomach, into the upper part of the small intestine to insert secretin and measure the response.
- Oral glucose tolerance test: You may need this test if your provider suspects that pancreatitis has damaged your insulin-producing pancreas cells. It measures how your body handles sugar with a blood test before and after you drink a sugary liquid.
- Stool test: Your provider may order a stool test using a sample of your stool to see if your body is having difficulty breaking down fat.
- Endoscopic ultrasound (endosonography): An internal (endoscopic) ultrasound takes clearer pictures of your pancreas and connecting ducts (tubes). A healthcare professional inserts a thin tube with a tiny ultrasound attachment into your throat, through your stomach and into your small intestine. The endoscopic ultrasound takes detailed pictures of your internal organs including pancreas, part of liver, gall bladder and bile duct.
- ERCP (endoscopic retrograde cholangiopancreatography): A tube with a tiny camera is passed from your throat to your stomach and into your small intestine up to the area called the ampulla, where the pancreas and bile duct opens. Dye is injected into the pancreas duct and /or bile duct. The test lets your provider see inside the pancreas and bile duct. Anything blocking the pancreas or bile duct, such as a gallstone or pancreas stone, may be removed.
Treatments
Doctors use one or more of these methods to treat acute pancreatitis:
- Hospitalization with supportive care and monitoring.
- Pain medication to provide comfort.
- Endoscopic procedure or surgery to remove a gallstone, other blockage or damaged part of the pancreas.
- Supplemental pancreatic enzymes and insulin, if your pancreas isn’t functioning well.
Procedures used to treat pancreatitis
Most pancreatitis complications like pancreatic pseudocyst (type of inflammatory cyst) or infected pancreas tissue are managed through endoscopic procedure (inserting a tube down your throat until it reaches your small intestine, which is next to your pancreas). Gallstones and pancreas stones are removed with an endoscopic procedure.
If surgery is recommended, surgeons can often perform a laparoscopic procedure.

Prevention
- Maintain a healthy weight.
- Get regular exercise.
- Stop smoking.
- Avoid alcohol.
These healthy lifestyle choices will also help you avoid gallstones, which cause 40% of acute pancreatitis cases. Your provider may recommend removing your gallbladder if you have painful gallstones multiple times.
Living With Pancreatitis
You can take several steps to prevent another pancreatitis attack:
- Eat a low-fat diet.
- Stop drinking alcoholic beverages.
- Quit smoking.
- Follow your doctor’s and nutritionist’s dietary recommendations.
• Take medications as prescribed.