Colon Cancer
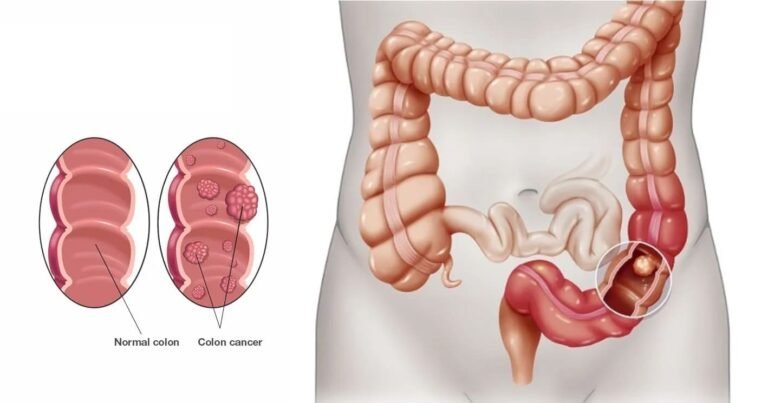
The large intestine is where colon cancer typically first manifests itself (colon). The digestive system ends with the colon.Colon cancer can affect anyone at any age, although it often affects older persons. Small, benign (noncancerous) cell clumps called polyps commonly grow on the inside of the colon as the first signs of the condition. Some of these polyps may eventually develop into colon cancer.Small polyps may have few, if any, symptoms. Because of this, medical professionals advise routine screening exams to help prevent colon cancer by locating and removing polyps before they transform into cancer.
There are several treatment available that can help treat colon cancer, such as surgery, radiation therapy, and medication such as chemotherapy, targeted therapy, and immunotherapy.The term colorectal cancer, which combines the terms colon cancer and rectal cancer (which starts in the rectum), is often used to refer to colon cancer.
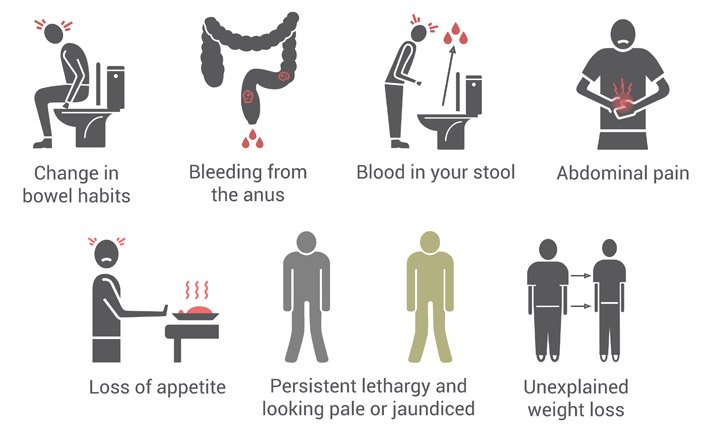
Signs & Symptoms
- A persistent change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool
- Rectal bleeding or blood in your stool
- Persistent abdominal discomfort, such as cramps, gas or pain
- A feeling that your bowel doesn’t empty completely
- Weakness or fatigue
- Unexplained weight loss
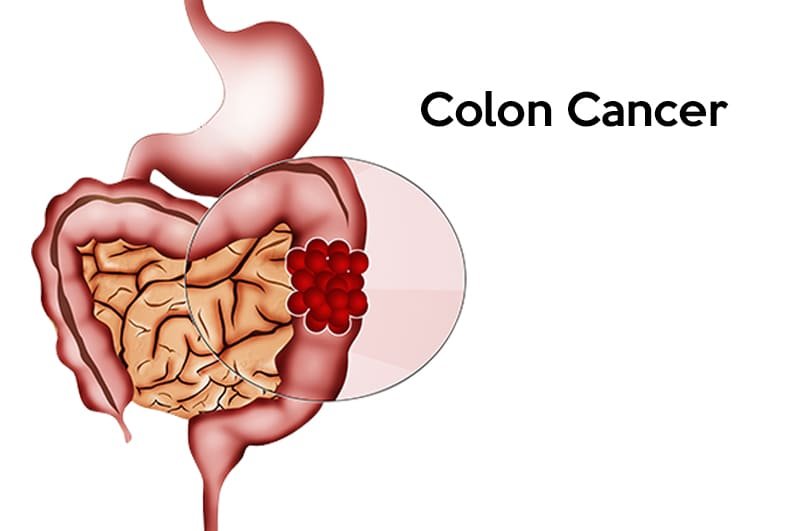
In general, colon cancer develops when healthy cells in the colon get DNA alterations. The DNA of a cell carries a collection of instructions that direct the cell what to do.
Healthy cells divide and expand in an ordered fashion to keep your body running smoothly. When a cell’s DNA is broken and it becomes malignant, it continues to divide — even when new cells aren’t required. As the cells multiply, they create a tumour.
Cancer cells can spread over time and infiltrate and kill normal tissue nearby. Furthermore, malignant cells might spread to other areas of the body and create deposits there (metastasis).
Risk factors
- Getting older. Colon cancer can be diagnosed at any age, however the majority of patients are over the age of 50. Colon cancer rates in persons under the age of 50 have been rising, but physicians aren’t sure why.
- African-American ethnicity African-Americans are more likely than other races to get colon cancer.
- Personal experience with colorectal cancer or polyps. If you’ve already had colon cancer or noncancerous colon polyps, you’re at a higher risk of developing colon cancer in the future.
- Inflammatory conditions of the intestine. Colon inflammatory illnesses, such as ulcerative colitis and Crohn’s disease, might raise your chance of developing colon cancer.

- Inherited disorders that raise the risk of colon cancer. Some DNA changes handed down through generations of your family can dramatically raise your risk of colon cancer. Only a tiny number of colon cancers have been related to hereditary genes. Familial adenomatous polyposis (FAP) and Lynch syndrome, often known as hereditary nonpolyposis colorectal cancer, are the most frequent inherited disorders that raise colon cancer risk (HNPCC).
- There is a family history of colon cancer. If you have a blood family who has had colon cancer, you are more likely to have it. If you have a family history of colon or rectal cancer, your risk is increased.
- A high-fat, low-fiber diet. A normal Western diet that is low in fibre and heavy in fat and calories may be linked to colon and rectal cancer. The outcomes of this research have been mixed. Some studies have discovered an elevated risk of colon cancer in persons who consume a lot of red and processed meat.
- A sedentary way of life. Inactive people are more prone to acquire colon cancer. Regular physical exercise may lower your chance of developing colon cancer.
- Diabetes. People who have diabetes or insulin resistance are at a higher risk of developing colon cancer.
- Obesity. Obese persons have a higher risk of colon cancer and a higher chance of dying from colon cancer when compared to people of normal weight.
- Smoking. People who smoke may be at a higher risk of developing colon cancer.
- Alcohol. Heavy alcohol use raises your chance of developing colon cancer.
- Cancer radiation treatment Radiation treatment to the abdomen for past tumours raises the risk of colon cancer.
Prevention
- Screening
Doctors advise persons with an average risk of colon cancer to begin colon cancer screening around the age of 45. People who are at a higher risk, such as those who have a family history of colon cancer, should consider screening sooner.
There are several screening options available, each with its own set of advantages and disadvantages. Discuss your choices with your doctor, and you can determine which tests are right for you.
Lifestyle changes to reduce your risk of colon cancer
- Consume a wide range of fruits, vegetables, and entire grains. Fruits, vegetables, and whole grains provide vitamins, minerals, fibre, and antioxidants that may help prevent cancer. Choose a variety of fruits and vegetables to ensure that you are getting a wide range of vitamins and minerals.
- Drink alcohol sparingly, if at all. If you prefer to drink alcohol, restrict your intake to no more than one drink per day for women and two drinks per day for men.
- Quit smoking. Consult your doctor about quitting methods that may be suitable for you.
- Most days of the week, exercise. On most days, try to obtain at least 30 minutes of exercise. If you’ve been inactive, begin cautiously and eventually up to 30 minutes. Also, before beginning any workout regimen, consult with your doctor.
- Keep a healthy weight. If you are already at a healthy weight, aim to keep it there by combining a nutritious diet with daily exercise. If you need to reduce weight, talk to your doctor about appropriate ways to do it. Aim to lose weight gradually by increasing your physical activity and decreasing your calorie intake.

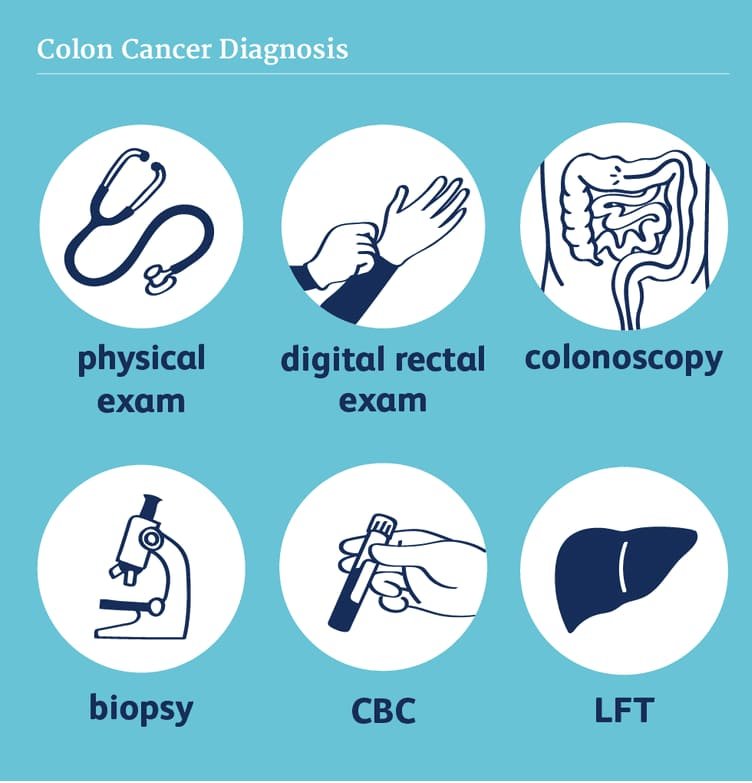
Diagnosis
- Colonoscopy
- Blood markers
- CT SCAN /MRI
Treatment
Early Stage of Colon Cancer
- Removing polyps during a colonoscopy (polypectomy). If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection. Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
- Minimally invasive surgery (laparoscopic surgery). Polyps that can’t be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
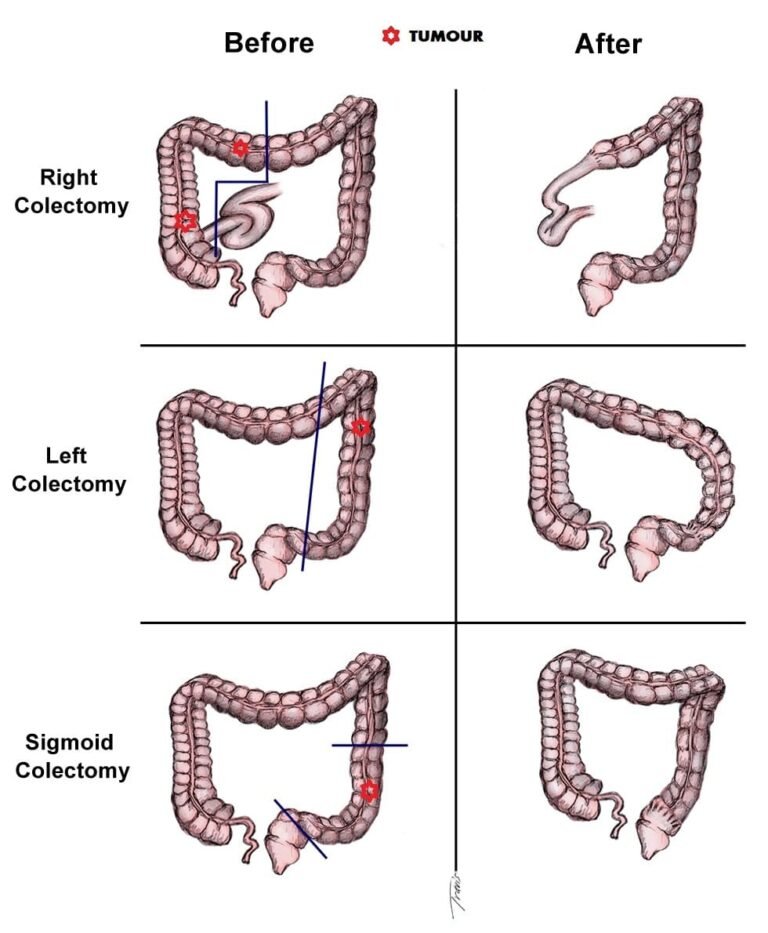
Surgery for More Advanced Colon Cancer
- Partial colectomy. During this procedure, the surgeon removes the part of your colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. Your surgeon is often able to reconnect the healthy portions of your colon or rectum. This procedure can commonly be done by a minimally invasive approach (laparoscopy).
- Surgery to create a way for waste to leave your body. When it’s not possible to reconnect the healthy portions of your colon or rectum, you may need an ostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
- Sometimes the ostomy is only temporary, allowing your colon or rectum time to heal after surgery. In some cases, however, the colostomy may be permanent.
Surgery for Advanced Cancer
- If your cancer is very advanced or your overall health very poor, your surgeon may recommend an operation to relieve a blockage of your colon or other conditions in order to improve your symptoms. This surgery isn’t done to cure cancer, but instead to relieve signs and symptoms, such as a blockage, bleeding or pain.
- In specific cases where the cancer has spread only to the liver or lung but your overall health is otherwise good, your doctor may recommend surgery or other localized treatments to remove the cancer. Chemotherapy may be used before or after this type of procedure. This approach provides a chance to be free of cancer over the long term.
Therapy
Chemotherapy
- Chemotherapy uses drugs to destroy cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is larger or has spread to the lymph nodes. In this way, chemotherapy may kill any cancer cells that remain in the body and help reduce the risk of cancer recurrence.
- Chemotherapy might also be used before an operation to shrink a large cancer so that it’s easier to remove with surgery.
- Chemotherapy can also be used to relieve symptoms of colon cancer that can’t be removed with surgery or that has spread to other areas of the body. Sometimes it’s combined with radiation therapy.
- For some people with low-risk stage III colon cancer, a shorter course of chemotherapy after surgery may be possible. This approach may reduce the side effects compared with the traditional course of chemotherapy, and may be just as effective.
Radiation Therapy
- Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. It might be used to shrink a large cancer before an operation so that it can be removed more easily.
- When surgery isn’t an option, radiation therapy might be used to relieve symptoms, such as pain. Sometimes radiation is combined with chemotherapy.
Targeted Drug Therapy
- Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
- Targeted drugs are usually combined with chemotherapy. Targeted drugs are typically reserved for people with advanced colon cancer.
Immunotherapy
- Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells from recognizing the cancer cells. Immunotherapy works by interfering with that process.
- Immunotherapy is usually reserved for advanced colon cancer. Your doctor might have your cancer cells tested to see if they’re likely to respond to this treatment.
Supportive (palliative) Care
- Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care is provided by a team of doctors, nurses and other specially trained professionals that work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
- Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
- When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer
- Lymph node removal. Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
