Pancreatic Cancer
Overview
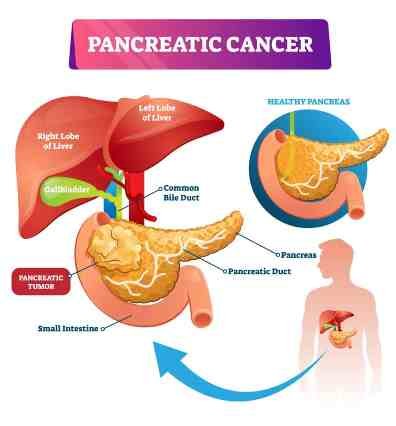
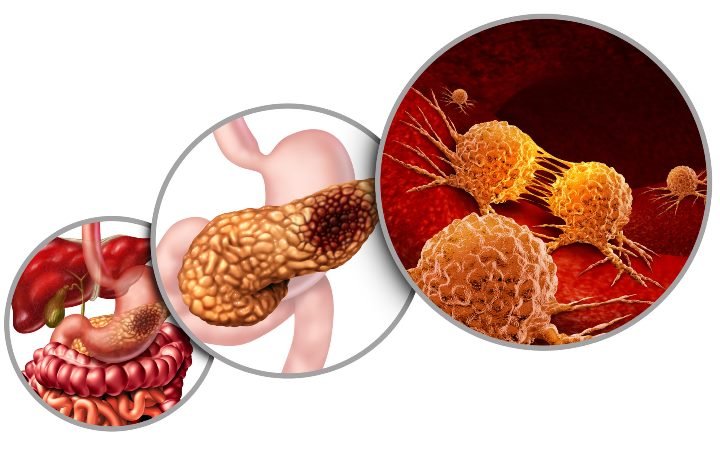
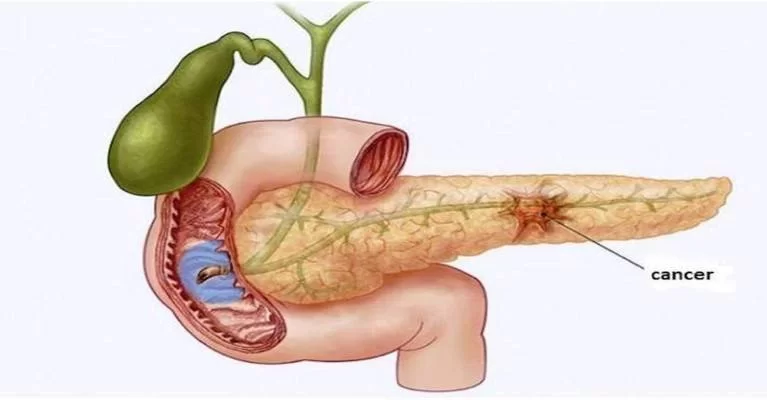
Pancreatic cancer occurs when changes (mutations) in the pancreas cells lead them to multiply out of control. A mass of tissue can result. Sometimes, this mass is benign (not cancerous). In pancreatic cancer, however, the mass is malignant (cancerous).
Types
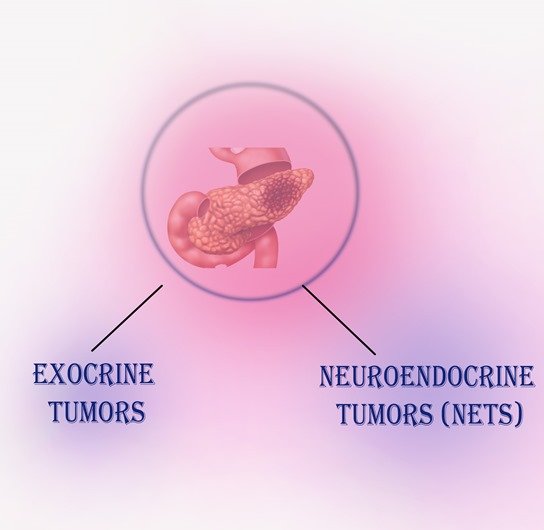
- Exocrine tumors
About 93% of all pancreatic tumors are exocrine tumors, and the most common kind of pancreatic cancer is called adenocarcinoma. Pancreatic adenocarcinoma is what people usually mean when they say they have pancreatic cancer. The most common type begins in the ducts of the pancreas and is called ductal adenocarcinoma.
- Neuroendocrine tumors (NETs)
about 7% of the total — are neuroendocrine tumors (NETs), also called pancreatic NETs (PNETs), an islet cell tumor or islet cell carcinoma. Some NETs produce excessive hormones. They may be called names based on the type of hormone the cell makes — for instance, insulinoma would be a tumor in a cell that makes insulin.
Risk Factors
- Smoking cigarettes, cigars and using other forms of tobacco.
- Obesity is also a risk factor. Carrying weight around the waist is a risk factor even if you do not have obesity.
- Having diabetes, especially type 2 diabetes, which is linked to obesity. The new development of diabetes at an older age and in someone with a normal weight or body mass index could be a sign of pancreatic cancer.
- Being exposed to chemicals used by dry cleaners and metal workers.
- Having chronic pancreatitis, a permanent inflammation of the pancreas usually associated with smoking and drinking a lot of alcohol.
Symptoms
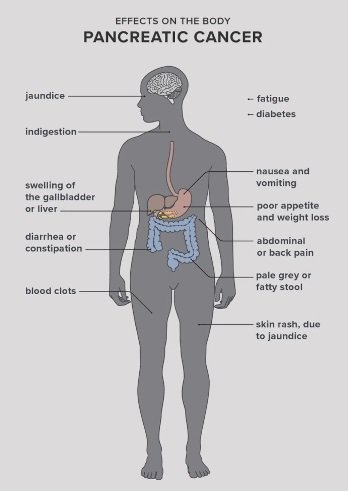
- Upper abdominal pain that may spread to the back.
- Yellowing of the skin and the whites of the eyes (jaundice).
- Tiredness.
- Loss of appetite.
- Light-colored poop.
- Dark-colored pee.
- Blood clots in the body.
- Itchy skin.
- New or worsening diabetes.
- Nausea and vomiting
Diagnosis
- Pancreatic cancer is difficult to detect in its early stages.
- This is due to the fact that healthcare practitioners cannot feel the pancreas during a typical checkup.If your doctor believes you have pancreatic cancer, he or she may prescribe imaging tests to acquire photographs of your internal organs. Endoscopic ultrasonography can also be performed.
- A narrow tube with a camera at the tip that is inserted through the mouth and into the stomach is known as an endoscopic ultrasonography (EUS). The endoscope’s ultrasonic probe permits imaging of the pancreatic through the stomach wall.
- During the process, an ultrasound guided biopsy (tissue sample) of the pancreas might be collected if necessary.
- A tumour marker can be detected in a blood test.
- High levels of carbohydrate antigen (CA) 19-9, a kind of protein secreted by pancreatic cancer cells, may indicate the presence of a tumour in pancreatic cancer.
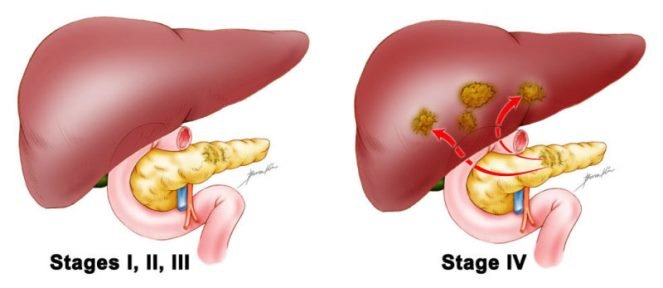
Stages of Pancreatic cancer
- Stage 0: Also known as carcinoma in situ, Stage 0 is characterized by abnormal cells in the lining of the pancreas. The cells could become cancerous and spread to nearby tissue.
- Stage 1: The tumor is in the pancreas.
- Stage 2: The tumor is in the pancreas and has either spread to nearby tissues, organs or lymph nodes.
- Stage 3: The cancer has spread to major blood vessels near the pancreas. It may have also spread to nearby lymph nodes.
- Stage 4: In stage 4 pancreatic cancer, the cancer has spread to distant areas in the body, such as the liver, lungs or abdominal cavity. It has possibly spread to organs, tissues or lymph nodes near the pancreas.
Treatment
Pancreatic cancer treatment depends on certain things, including where the tumor is located, what stage it is in, how healthy you are and whether or not the cancer has spread beyond the pancreas. Treatment options include:
- Surgical removal: The cancerous part of the pancreas (resection) is removed. Lymph nodes near to the pancreas may also be removed. The surgery to remove the pancreas or part of the pancreas is called a pancreatectomy. If your tumor is located in the head (the widest part of pancreas near small intestine) of the pancreas, your provider may recommend the Whipple procedure. This surgical method removes the head of the pancreas, the duodenum (the first portion of the small intestine), the gallbladder, a portion of the bile duct and nearby lymph nodes.
- Radiation therapy: High-speed energy used to kill the cancer cells.
- Chemotherapy: This method uses drugs that kill cancer cells.
- Immunotherapy: Treatment to help your body fight the cancer. Immunotherapy has largely been ineffective against pancreatic cancer, but about 1% of people with pancreatic cancer and a specific genetic change may benefit from it.
- Targeted therapy: Directed at certain genes or proteins that help cancer grow. Genetic testing is generally how we determine if a targeted therapy is right for you.
Palliative Care in Advance Cancer
- Pain management: If pain medication fails to provide relief, an endoscopic procedure called celiac plexus block or neurolysis can be performed under direct guidance from endoscopic ultrasound.
- Jaundice treatment: Your healthcare provider can insert a stent (tube) inside your bile duct to manage your jaundice symptoms.
- Reducing intestinal blockage: Your provider can insert a stent to open up the blockage in your small intestine.
- Diabetes control: Your medical team can help monitor your blood sugar levels and manage your diabetes medicine.
- Emotional support: Supportive care can also help you understand and process your own emotions and those of your family and friends.
- In stage 4 pancreatic cancer, the cancer has spread to distant areas in the body, such as the liver, lungs or abdominal cavity. It has possibly spread to organs, tissues or lymph nodes near the pancreas.
Prevention
- Don’t smoke. If you do smoke or use tobacco in any form, try to quit.
- Try to reach and maintain a normal weight by eating healthy and exercising.
- Drink alcohol in moderation, or quit drinking altogether.
- Try to avoid getting diabetes. If you have it, control your blood sugar levels.
- Use safety equipment if your work exposes you to toxins.
